order histories, retained contact details for faster checkout, review submissions, and special promotions.
Forgot password?
order histories, retained contact details for faster checkout, review submissions, and special promotions.
Location
Corporate Headquarters
Vector Laboratories, Inc.
6737 Mowry Ave
Newark, CA 94560
United States
Telephone Numbers
Customer Service: (800) 227-6666 / (650) 697-3600
Contact Us
Additional Contact Details
order histories, retained contact details for faster checkout, review submissions, and special promotions.
Forgot password?
order histories, retained contact details for faster checkout, review submissions, and special promotions.
Post COVID-19 Coronary Implications
By Vagmita Pabuwal and Samia Ahmed
LifeSpan Biosciences, Inc.
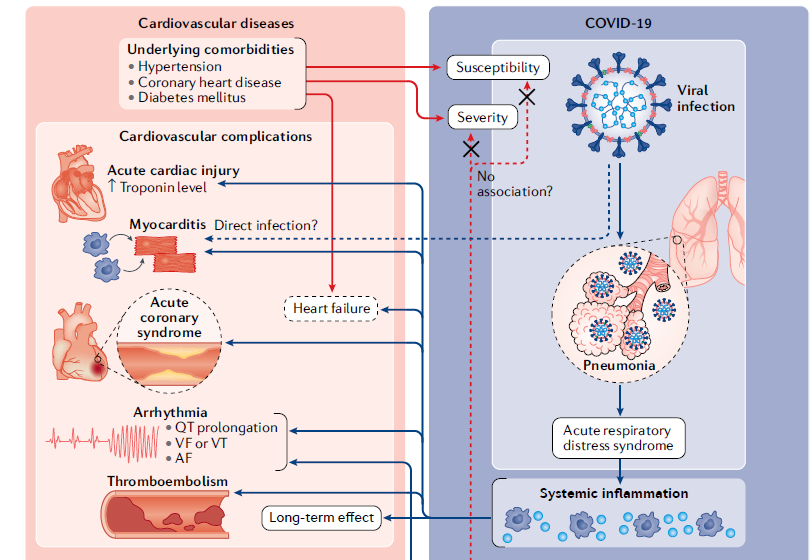
After over a year of studying the Sars-CoV-2 virus, mounting evidence is suggesting a number of post COVID-19 coronary implications in some patients. Nearly 25% of those hospitalized with COVID-19 have been diagnosed with cardiovascular complications. Some of these complications can lead to an increase in chance of heart failure at a later point in time, even after the patient seems to be recovering from the initial illness. Cardiovascular disorders can include myocardial injury, arrhythmias, acute coronary syndrome heart failure, and venous thromboembolism. Progression in cardiovascular damage in COVID-19 is associated with general systemic inflammation. Acute hypoxic respiratory failure is the hallmark of severe COVID-19, with arrhythmias and sudden cardiac arrest being other common observations. Individuals with pre-existing cardiovascular disease and/or development of acute cardiac injury are generally associated with significantly worse outcomes.
The interaction between the viral spike (S) protein and angiotensin-converting enzyme 2(ACE2) is likely to be involved in the cardiovascular manifestations of COVID-19. The primary function of ACE2 as a peptidase is the metabolism of angiotensin II (ANG II) to angiotensin 1-7 (ANG-(1-7)). The binding of ACE2 to SARS-CoV-2 prevents metabolism and leads to an increased ANG II to ANG-(1-7) ratio, which is detrimental to cardiac function. ACE2 peptidase is expressed in type II alveolar cells, stratified epithelial cells of the upper airway and esophagus, enterocytes of the ileum and colon, myocardial cells, vascular endothelial cells, proximal tubules of the kidney, and urothelial cells. This explains the multi-organ involvement of this infection far beyond the alveolar cells of the lungs, including the cardiovascular system. Future research will undoubtedly be needed to fully understand the long term implications of COVID-19 cardiac effects.
Listed below are the possible cardiovascular abnormalities and manifestations associated with them:
Acute cardiac injury: Identified by significantly elevated levels of cardiac troponins. It is the most commonly reported cardiac abnormality in COVID-19. High-sensitivity troponin I was significantly elevated in over half of fatal COVID-19 cases. Direct myocardial injury due to viral involvement of cardiomyocytes and the effect of systemic inflammation appear to be the most common mechanisms responsible for cardiac injury (Nishiga, M et.al 2020).
Myocarditis: Myocarditis is identified by segmental wall motion abnormality or reduced left ventricular ejection fraction. In patients where ECG/EKG did not have these typical signs, suggesting that observed myocardial injury was secondary to systemic causes rather than direct effect on heart due to viral infection. (Nishiga, M et.al 2020).
Acute coronary syndrome: Although the mechanism underlying covid-19 induced ACS might involve plaque rupture, coronary spam or thrombi due to systemic inflammation or cytokine storm, ACS is observed in individuals even without the presence of substantial systemic inflammation. Direct endothelial or vascular injury caused by SARS-CoV-2 infection might also increase the risk of thrombus formation and ACS (Varga, Z. 2020). Acute myocardial injury and ACS triggered by COVID-19 can also aggravate pre-existing heart disease or provoke contractile dysfunction. Stress- induced cardiomyopathy or cytokine- related myocardial dysfunction, can be triggered in advanced covid-19 as seen with sepsis- associated cardiac dysfunction due to increased immune response towards infection. (Fried, J.A 2020) (Prabhu, 2004).
Heart Failure: Heart failure (HF) is a clinical syndrome caused by structural and functional defects in myocardium resulting in impairment of ventricular filling or the ejection of blood (Inamdar, A.A 2016). Elevated level of amino- terminal pro- B- type natriuretic peptide was observed, indicating of increased pressure on heart (Nishiga, M et.al 2020). In particular, elderly patients with reduced diastolic function might develop heart failure, which can be triggered by high fever, tachycardia, excessive hydration and impaired renal function.
Arrhythmia and sudden cardiac arrest: Arrhythmias and sudden cardiac arrest are common manifestations of COVID-19. Heart palpitations are reported to be the main presenting symptom of COVID-19 in patients without a fever or cough. Elevated levels of troponin T were more likely to develop malignant arrhythmias 24. It is hypothesized that myocardial injury, systemic causes such as fever, sepsis, hypoxia and electrolyte abnormalities can cause cardiac arrhythmias (Nishiga, M et.al 2020).
Coagulation abnormalities and thrombosis: COVID-19 is associated with coagulation abnormalities, which can result in thromboembolic events. Patients with COVID-19 often have elevated levels of d- dimer indicating reduced platelet counts and slightly prolonged prothrombin time. Higher level of d-dimer is directly associated with severity of covid-19. High levels of fibrinogen and factor VIII, in COVID-19 patients indicate a hypercoagulable state. Coagulation abnormalities might contribute to the development of the diverse cvd manifestations of covid-19. Venous thromboembolism, which includes deep vein thrombosis and pulmonary embolism, is a common complication in critically ill patients with COVID-19 (Nishiga, M et.al 2020).
The majority of the COVID-19 patients suffering from cardiovascular complications show a significant elevation of cTnI, NT-proBNP and interleukin-6 (IL-6) or other cytokines [IL1B, IL1RA, IL7, IL8, IL9, IL10, C-X-C motif chemokine 10 (CXCL10), chemokine (C-C motif) ligand 2 (CCL2), granulocyte-macrophage colony-stimulating factor (GM-CSF), and tumor necrosis factor-α (TNF-α)] in their blood stream.
The following targets are directly involved in cardiac abnormalities:
ACE2, or Angiotensin-Converting Enzyme 2, plays a central role in vascular, renal, and myocardial physiology. In contrast to its homolog ACE, ACE2 expression is restricted to heart, kidney, and testis. The normal function of ACE2 is to convert the inactive vasoconstrictor angiotensin I (AngI) to Ang1-9 and the active form AngII to Ang1-7, unlike ACE, which converts AngI to AngII. While the role of these vasoactive peptides is not well understood, lack of ACE2 expression in ace2-/ace2- mice leads to severely reduced cardiac contractility, indicating its importance in regulating heart function.
TNNT2 / CTNT is the tropomyosin-binding subunit of the troponin complex, which is located on the thin filament of striated muscles and regulates muscle contraction in response to alterations in intracellular calcium ion concentration. Mutations in this gene have been associated with familial hypertrophic cardiomyopathy as well as with dilated cardiomyopathy.
NPR3 is the receptor for the natriuretic peptide hormones, binding with similar affinities atrial natriuretic peptide NPPA/ANP, brain natriuretic peptide NPPB/BNP, and C-type natriuretic peptide NPPC/CNP. May function as a clearance receptor for NPPA, NPPB and NPPC, regulating their local concentrations and effects. May regulate diuresis, blood pressure and skeletal development.
References
- Babapoor-Farrokhran, S., Gill, D., Walker, J., Rasekhi, R. T., Bozorgnia, B., & Amanullah, A. (2020). Myocardial injury and COVID-19: Possible mechanisms. Life Sciences, 253, 117723. https://doi.org/10.1016/j.lfs.2020.117723
- Bansal, M. (2020). Cardiovascular disease and COVID-19. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(3), 247–250. https://doi.org/10.1016/j.dsx.2020.03.013
- Blomfield, D., & Futter, M. (1989). Peripheral nerve stimulator. Anaesthesia and Intensive Care, 17(3), 380–381.
- Dassanayaka, S., & Jones, S. P. (2015). Recent Developments in Heart Failure. Circulation Research, 117(7). https://doi.org/10.1161/CIRCRESAHA.115.305765
- Fried, J. A., Ramasubbu, K., Bhatt, R., Topkara, V. K., Clerkin, K. J., Horn, E., Rabbani, L., Brodie, D., Jain, S. S., Kirtane, A. J., Masoumi, A., Takeda, K., Kumaraiah, D., Burkhoff, D., Leon, M., Schwartz, A., Uriel, N., & Sayer, G. (2020). The Variety of Cardiovascular Presentations of COVID-19. Circulation, 141(23), 1930–1936. https://doi.org/10.1161/CIRCULATIONAHA.120.047164
- Inamdar, A. A., & Inamdar, A. C. (2016). Heart Failure: Diagnosis, Management and Utilization. Journal of Clinical Medicine, 5(7). https://doi.org/10.3390/jcm5070062
- Libby, P., Tabas, I., Fredman, G., & Fisher, E. A. (2014). Inflammation and its resolution as determinants of acute coronary syndromes. Circulation Research, 114(12), 1867–1879. https://doi.org/10.1161/CIRCRESAHA.114.302699
- Mahenthiran, A. K., Mahenthiran, A. K., & Mahenthiran, J. (2020). Cardiovascular system and COVID-19: Manifestations and therapeutics. Reviews in Cardiovascular Medicine, 21(3), 399. https://doi.org/10.31083/j.rcm.2020.03.124
- Nishiga, M., Wang, D. W., Han, Y., Lewis, D. B., & Wu, J. C. (2020). COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nature Reviews Cardiology, 17(9), 543–558. https://doi.org/10.1038/s41569-020-0413-9
- Prabhu, S. D. (2004). Cytokine-Induced Modulation of Cardiac Function. Circulation Research, 95(12), 1140–1153. https://doi.org/10.1161/01.RES.0000150734.79804.92
- Varga, Z., Flammer, A. J., Steiger, P., Haberecker, M., Andermatt, R., Zinkernagel, A. S., Mehra, M. R., Schuepbach, R. A., Ruschitzka, F., & Moch, H. (2020). Endothelial cell infection and endotheliitis in COVID-19. The Lancet, 395(10234), 1417–1418. https://doi.org/10.1016/S0140-6736(20)30937-5
- Xu, H., Zhong, L., Deng, J., Peng, J., Dan, H., Zeng, X., Li, T., & Chen, Q. (2020). High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. International Journal of Oral Science, 12(1), 8. https://doi.org/10.1038/s41368-020-0074-x
- Yahia, F., Zakhama, L., & Ben Abdelaziz, A. (2020). COVID-19 and Cardiovascular diseases. Scoping review study. La Tunisie Medicale, 98(4), 283–294.